Ozempic (Semaglutide) Product Information: SPC, PI, Leaflet, and Instructions
Ozempic® (semaglutide) is one of the most widely prescribed GLP-1 receptor agonists for the treatment of type 2 diabetes and weight management. If you are considering starting this medication in France, Germany, the UK, the Netherlands, or elsewhere in Europe, it’s essential to understand its official prescribing information, packaging, instructions, and dosing guidance.
This page provides an easy-to-read summary of the Ozempic SPC (Summary of Product Characteristics), Prescribing Information (PI), patient leaflet, and common FAQs.
🔹 1. What is Ozempic?
Ozempic contains the active substance semaglutide, a GLP-1 analogue that works by:
-
Stimulating insulin secretion when blood sugar is high
-
Reducing appetite and slowing gastric emptying
-
Supporting long-term weight loss in patients with diabetes or obesity
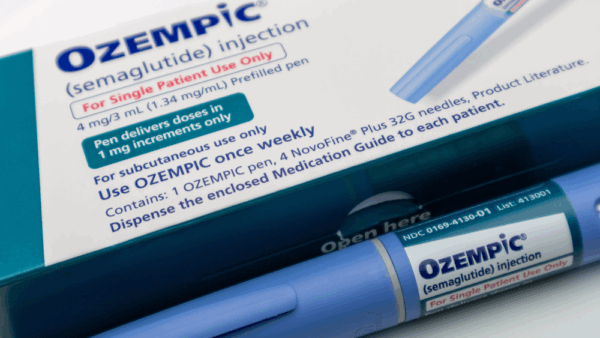
Ozempic is available as a prefilled injection pen for subcutaneous (under the skin) injection.
👉 For alternatives, see our full weight loss medications guide.
🔹 2. Ozempic Indications
According to the official Ozempic prescribing information (PI):
-
Type 2 diabetes mellitus – to improve blood sugar control in adults, either alone or with other medications.
-
Weight management – increasingly prescribed off-label or via Wegovy, which contains the same active ingredient in higher doses.
💡 Not indicated for type 1 diabetes or patients with diabetic ketoacidosis.
🔹 3. Dosage & Administration
Starting dose:
-
0.25 mg once weekly for 4 weeks (for tolerance).
Step-up dosing:
-
Increase to 0.5 mg weekly, then if needed to 1 mg weekly.
-
Some patients may use 2 mg pens depending on clinical need.
👉 Many users ask if you can start Ozempic at 1 mg — the answer is no. Starting at 1 mg increases side effects (nausea, vomiting, diarrhea). Always begin at 0.25 mg and titrate slowly.
For specific details, see the Ozempic dosage instructions page.
🔹 4. Ozempic 1 mg and 4 mg Pens
Ozempic pens are available in several strengths:
-
Ozempic 1 mg pen – common maintenance dose
-
Ozempic 2 mg or 4 mg pens – allow for higher dosing with fewer injections
Each pen comes with single-use NovoFine® needles, though patients may also purchase replacement needles separately.
🔹 5. Method of Administration: Is Ozempic Subcutaneous?
Yes. Ozempic is injected subcutaneously (under the skin), never intravenously or intramuscularly.
Recommended injection sites:
-
Abdomen
-
Thigh
-
Upper arm
Rotate sites each week to minimize irritation.
For a step-by-step visual, check the official Ozempic instructions PDF (IFU) included with each pen.
🔹 6. SPC, PI, and Patient Leaflet
Patients and healthcare professionals often search for different types of documentation:
-
SPC (Summary of Product Characteristics): Detailed medical information for doctors.
-
PI (Prescribing Information): U.S. equivalent of SPC, with clinical trial data, warnings, and interactions.
-
Leaflet: Patient-friendly version included in the packaging.
-
IFU (Instructions for Use): Pen-specific guidance with illustrations.
👉 We recommend always reading the leaflet and IFU carefully before use.
🔹 7. Packaging & Storage
Each Ozempic package contains:
-
Prefilled disposable pens (varies by strength)
-
Disposable pen needles
-
Patient leaflet with instructions
Storage:
-
Unopened pens: refrigerate at 2–8°C.
-
After opening: keep at room temperature (below 30°C) or refrigerated, for up to 6 weeks.
🔹 8. Common Side Effects
The most frequent Ozempic side effects include:
-
Nausea
-
Vomiting
-
Diarrhea
-
Constipation
-
Reduced appetite
These effects usually improve after the dose is stabilized. For patients with thyroid history, review our article on semaglutide and hypothyroidism.
🔹 9. Internal Resources
For further details, explore:
✅ Conclusion
Understanding the official product information for Ozempic ensures safe and effective use. From SPC and PI data to patient leaflets and injection instructions, knowing how the medication works helps patients in Europe and worldwide get the most out of treatment.
👉 To learn more or purchase, visit our Ozempic product page.
Tab Title
Find Ozempic Near Me: Navigating Availability and Access
The search “Ozempic near me” is one of the most common and frustrating steps for individuals seeking this in-demand medication. With frequent supply shortages, finding pharmacies with Ozempic in stock can feel like a challenge. At SemaglutidePourTous, we understand this struggle and aim to provide practical solutions for patients across Europe. This guide will help you navigate the search for “where to get Ozempic near me” and introduce a reliable alternative.
Why Is It So Hard to Find Ozempic?
Before you start calling every pharmacy, it’s important to understand the context. Ozempic and similar GLP-1 medications have seen unprecedented global demand, far exceeding manufacturing capabilities. This has led to widespread shortages, making a simple search for “Ozempic availability near me” often yield disappointing results. Regulatory bodies like the European Medicines Agency (EMA) regularly publish updates on medicine shortages, and Ozempic has frequently been on these lists.
How to Check “Ozempic Near Me”: A Step-by-Step Guide
If you are looking for local Ozempic pharmacies, here is the most effective strategy:
-
Get a Valid Prescription First: This is the non-negotiable first step. You cannot purchase Ozempic without a prescription from a licensed healthcare provider. Your search for “where can I find Ozempic in stock near me” must begin in your doctor’s office.
-
Call Pharmacies Directly: Once you have your prescription, start calling pharmacies. Larger chain pharmacies often have more buying power but also more patients. Don’t neglect smaller, independent pharmacies, as they can sometimes have stock when larger chains are depleted.
-
Ask the Right Questions: When you call, be specific. Ask: “Do you currently have Ozempic [your specific dose, e.g., 1mg] in stock?” Be prepared to provide your prescription details if they have it.
-
Be Persistent and Patient: Stock can arrive any day of the week. You may need to call back multiple times. Pharmacists are incredibly busy, so being polite and patient will get you further.
-
Consider Pharmacy Availability Brokers: Some regions have online platforms or apps that aggregate stock information from multiple pharmacies. Check if such a service exists in your country.
The Challenges of the Local Pharmacy Search
While the traditional method is to find a local pharmacy, this path has significant hurdles:
-
Time-Consuming: You may spend hours calling dozens of pharmacies.
-
Unreliable: Stock information can change by the minute. A pharmacy that has stock when you call might sell out before you arrive.
-
Geographically Limiting: You are restricted to your immediate area, which severely limits your options during a widespread shortage.
A Reliable Alternative: Online Access with SemaglutidePourTous
For many patients across Europe, the endless search for “Ozempic near me” is no longer the only option. SemaglutidePourTous offers a streamlined, reliable alternative that bypasses the frustration of local pharmacy shortages.
How it works:
-
Online Consultation: Complete a comprehensive online medical questionnaire which is reviewed by a licensed European healthcare professional.
-
Electronic Prescription: If you are deemed a suitable candidate, a prescription is issued electronically.
-
Direct Delivery: We partner with licensed and accredited pharmacies across the EU to dispense and ship genuine, approved medication directly to your door, often within a few days.
Benefits of this approach:
-
No More Stock Anxiety: We manage the supply chain, so you don’t have to. We work with multiple pharmacies to source medication.
-
Convenience: Everything is handled online, saving you time and effort.
-
European-Wide Access: Your options are not limited by your zip code. We serve patients across multiple European countries.
-
Continuity of Care: We ensure you have ongoing support and guidance, not just a one-time transaction.
Ensuring You Get Genuine Medication
Whether you find a local pharmacy or use our service, ensuring you receive authentic Ozempic is paramount. Always check that:
-
The packaging is sealed and has the correct branding.
-
The medication is within its expiration date.
-
You are using a licensed distributor or pharmacy. You can verify a pharmacy’s credentials through national regulatory bodies like the General Pharmaceutical Council (GPhC) in the UK, or its equivalent in your EU country.
Conclusion: From “Near Me” to “Delivered to Me”
The search for “Ozempic near me” is a symptom of a larger supply and demand issue. While checking local pharmacies with Ozempic in stock is a valid approach, it is often fraught with challenges.
For a predictable, convenient, and reliable path to access, consider modern solutions. SemaglutidePourTous provides a secure platform that connects eligible European patients with licensed doctors and pharmacies, turning the stressful quest for medication into a simple, managed process.
How to Buy Semaglutide in the UK: A Safe Access Guide for 2025-2026
Searches like “semaglutide buy uk” and “where can i buy semaglutide uk” have surged as awareness of this effective treatment grows. However, navigating the market safely is paramount. At SemaglutidePourTous, we are committed to ensuring patients in the UK and across Europe can access genuine medication through legal and secure channels. This guide will walk you through the legitimate routes to access semaglutide in the UK and what to avoid.
Understanding the Legal Landscape in the UK
In the UK, semaglutide (the active ingredient in Ozempic and Wegovy) is a prescription-only medication (POM). This means it is illegal to sell or supply it without a valid prescription from a qualified prescriber. It is also illegal to advertise prescription medicines directly to the public. Therefore, any website openly offering to “buy Ozempic UK” without first conducting a medical consultation is operating illegally and likely selling counterfeit or unsafe products.
The Medicines and Healthcare products Regulatory Agency (MHRA), the UK’s regulatory body, strictly enforces these rules to protect public health.
Tab Title
The Dangers of Illicit Online Markets
The high demand and cost have led to a dangerous black market. Searching for “semaglutide buy uk” can lead you to illicit online pharmacies, social media sellers, or websites offering “generic” or “compounded” semaglutide.
These sources pose severe risks:
-
Counterfeit Products: The medication may contain no active ingredient, the wrong dose, or harmful contaminants.
-
No Medical Oversight: You will not have a doctor to screen for contraindications (e.g., thyroid cancer history) or to manage side effects.
-
Legal Repercussions: Importing a prescription medicine without a valid prescription is illegal.
The National Pharmacy Association (NPA) consistently warns patients about the dangers of buying prescription medicines online from unverified sources.
How to Safely Access Semaglutide in the UK
There are two primary legitimate pathways to access semaglutide:
1. The NHS Route:
-
Ozempic® is licensed for treating type 2 diabetes. Its use on the NHS is subject to strict NICE guidelines and may be restricted based on local CCG (Clinical Commissioning Group) formularies.
-
Wegovy® (a higher-dose semaglutide injection for weight loss) received UK approval. However, its availability on the NHS is extremely limited and typically reserved for specialist weight management services within specific criteria. The NHS website provides information on available weight management treatments.
2. The Private Healthcare Route:
This is the most common route for individuals seeking treatment for weight loss. This involves:
-
Private GP or Clinic: Having a consultation with a private doctor or a specialist weight loss clinic. If you are a suitable candidate, they will issue a private prescription.
-
Filling the Prescription: You can then take this prescription to a pharmacy. This leads to the related search for “ozempic injections near me” or “ozempic shots near me“. You would need to find a local pharmacy that stocks the medication and is willing to dispense a private prescription.
The Challenge of “Ozempic Injections Near Me”
The search for “ozempic injections near me” highlights a key frustration: even with a valid prescription, supply shortages can make it difficult to find a pharmacy with stock. Patients often must call multiple pharmacies, a time-consuming and often disappointing process.
A Secure and Convenient Alternative: SemaglutidePourTous
For UK patients seeking a reliable solution beyond searching “ozempic shots near me“, SemaglutidePourTous offers a safe, online-based private healthcare service.
Our process ensures full compliance and safety:
-
UK-Friendly Online Consultation: Our platform connects you with registered European healthcare professionals who can conduct a remote assessment. They will evaluate your medical history to determine if semaglutide is appropriate for you.
-
Legitimate Prescription: If approved, a legal prescription is issued.
-
Dispensing by Licensed Pharmacies: We work exclusively with licensed and regulated pharmacies within the EU that can dispense genuine, MHRA-approved medication.
-
Direct, Discreet Delivery: Your medication is delivered directly to your door in the UK, eliminating the need to physically search for stock.
We provide a seamless alternative to the stressful and often unsuccessful search to “buy semaglutide uk” from unknown sources.
Key Takeaways for UK Patients
-
Never buy semaglutide without a prescription. It is illegal and dangerous.
-
Avoid websites that offer to sell it without a consultation. This is a major red flag.
-
Understand that NHS access is limited to specific medical criteria.
-
Private prescription is the standard route for weight management treatment.
-
Using a reputable service like SemaglutidePourTous ensures you get genuine medication with necessary medical oversight.
Conclusion: Prioritise Safety Over Speed
While the desire to quickly “buy Ozempic UK” is understandable, your health must come first. The safest way to obtain semaglutide is through a regulated healthcare pathway that includes a medical consultation, a legitimate prescription, and a licensed pharmacy.
Product information
Tab Title
Ozempic Product Information: Prescribing Guidance, SPC, Leaflet, and Dosing
Ozempic® (semaglutide) is one of the most prescribed GLP-1 receptor agonists for managing type 2 diabetes and supporting weight loss in adults across Europe, including France, Germany, the UK, and the Netherlands. Patients and clinicians often search for clear details about the semaglutide SPC, Ozempic PI (Prescribing Information), leaflet, IFU (Instructions for Use), packaging, and dosage. This comprehensive guide provides all essential product information, explained in plain language.
What is Ozempic?
Ozempic contains semaglutide, a GLP-1 analogue that helps lower blood sugar, reduce appetite, and support weight reduction. It comes in prefilled injection pens designed for subcutaneous use, usually once per week.
Unlike traditional diet pills or stimulants such as Phentermine, Ozempic works on gut-hormone pathways and offers longer-term metabolic benefits.
For a broader look at prescription options, see our weight loss medications guide.
Ozempic Indications
According to the official Ozempic indications:
-
To improve glycemic control in adults with type 2 diabetes
-
To reduce risk of major cardiovascular events in patients with both diabetes and heart disease
-
Increasingly prescribed for weight loss, either off-label or under its higher-dose brand, Wegovy
It is not recommended for patients with type 1 diabetes or diabetic ketoacidosis.
Dosage and Administration
Standard dosing schedule:
-
Begin with 0.25 mg once weekly for 4 weeks
-
Increase to 0.5 mg weekly
-
Escalate to 1 mg weekly, if needed
Some patients progress to 2 mg pens. Newer packaging also includes Ozempic 4 mg pens for extended dosing with fewer injections.
Can you start Ozempic at 1 mg? No — treatment must begin at 0.25 mg to minimize gastrointestinal side effects.
Patients interested in oral therapy may prefer Rybelsus (oral semaglutide).
Method of Administration
Is Ozempic subcutaneous? Yes. It should always be injected just beneath the skin, never intravenously.
Common injection sites include:
-
Abdomen
-
Thigh
-
Upper arm
Rotate the site each week. For step-by-step visuals, see the Ozempic Instructions for Use (IFU) or download the Ozempic pen instructions PDF.
Packaging and Storage
Each package typically includes:
-
Prefilled disposable pens (strength varies by prescription)
-
Disposable NovoFine® needles
-
Patient leaflet and detailed instructions PDF
Storage guidelines:
-
Keep unopened pens refrigerated at 2–8°C
-
Once in use, store at room temperature (below 30°C) or refrigerated for up to 6 weeks
For patients comparing options, our Mounjaro page offers insights into how tirzepatide is packaged differently.
SPC, PI, Leaflet, and Prescribing Information
Healthcare professionals may request different documents:
-
Semaglutide SPC (Summary of Product Characteristics): Full technical data on pharmacology and interactions
-
Ozempic PI (Prescribing Information): U.S. equivalent of the SPC, with trial results and dosage tables
-
Ozempic leaflet: Patient-friendly version included in every box
-
Ozempic IFU: Pen instructions with illustrated guidance
Digital formats such as the Ozempic prescribing information PDF are available from manufacturers and pharmacies.
Side Effects and Warnings
The most common side effects are gastrointestinal:
-
Nausea
-
Vomiting
-
Diarrhea
-
Constipation
-
Loss of appetite
Less frequent risks include gallbladder issues and, rarely, thyroid tumors. Patients with thyroid disorders should read our full guide on semaglutide and hypothyroidism.
Clinical Alternatives
Patients may also consider:
-
Saxenda (liraglutide) – another GLP-1 agonist for weight management
-
Contrave – combination therapy targeting cravings
-
Phentermine – a stimulant appetite suppressant still used in some European countries
All are available in our weight loss medications category.
Additional Resources
For broader learning, explore:
-
All products are available in our online pharmacy
-
Blog section for news and weight management tips
-
Checkout via our secure order page
-
Reach us via Contact page if you need prescription support
Conclusion
Ozempic has become a cornerstone of modern diabetes and weight management therapies. By reviewing the SPC, PI, leaflet, and IFU, patients across France, Germany, the UK, and the Netherlands can better understand safe use, dosing, and storage.
For treatment details, dosage adjustments, and product availability, visit our Ozempic product page or consult with your prescribing doctor.